Artificial skin with natural blood vessels
The generation of new blood vessels, angiogenesis, plays an important role in medicine. Inhibiting angiogenesis for example helps to slow down tumor growth, whilst in wound healing processes angiogenesis should be stimulated. In her university thesis carried out at the Fraunhofer IGB, Silke Kersen has investigated, how blood vessels can be created in an artificial skin equivalent. She built the first human 3D skin model with capillary-like structures. It can be applied in tumor research and as well be developed further to a well-supplied skin transplant.
Animal experiments are being increasingly replaced by pharmacological tests on tissues cultivated in the laboratory. The artificial tissues are at the same time becoming more complex, and this benefits organ transplants. Whereas artificial skin initially consisted of simple cell collections of a single type, models can be generated today that represent the various layers of the skin and incorporate capillary-like structures – the precursors of blood vessels. Such models are also of interest in basic research, as they permit the investigation of key oncological questions: Why, in many tumors, does the highly branched blood system grow so quickly, and how can this growth be slowed down?
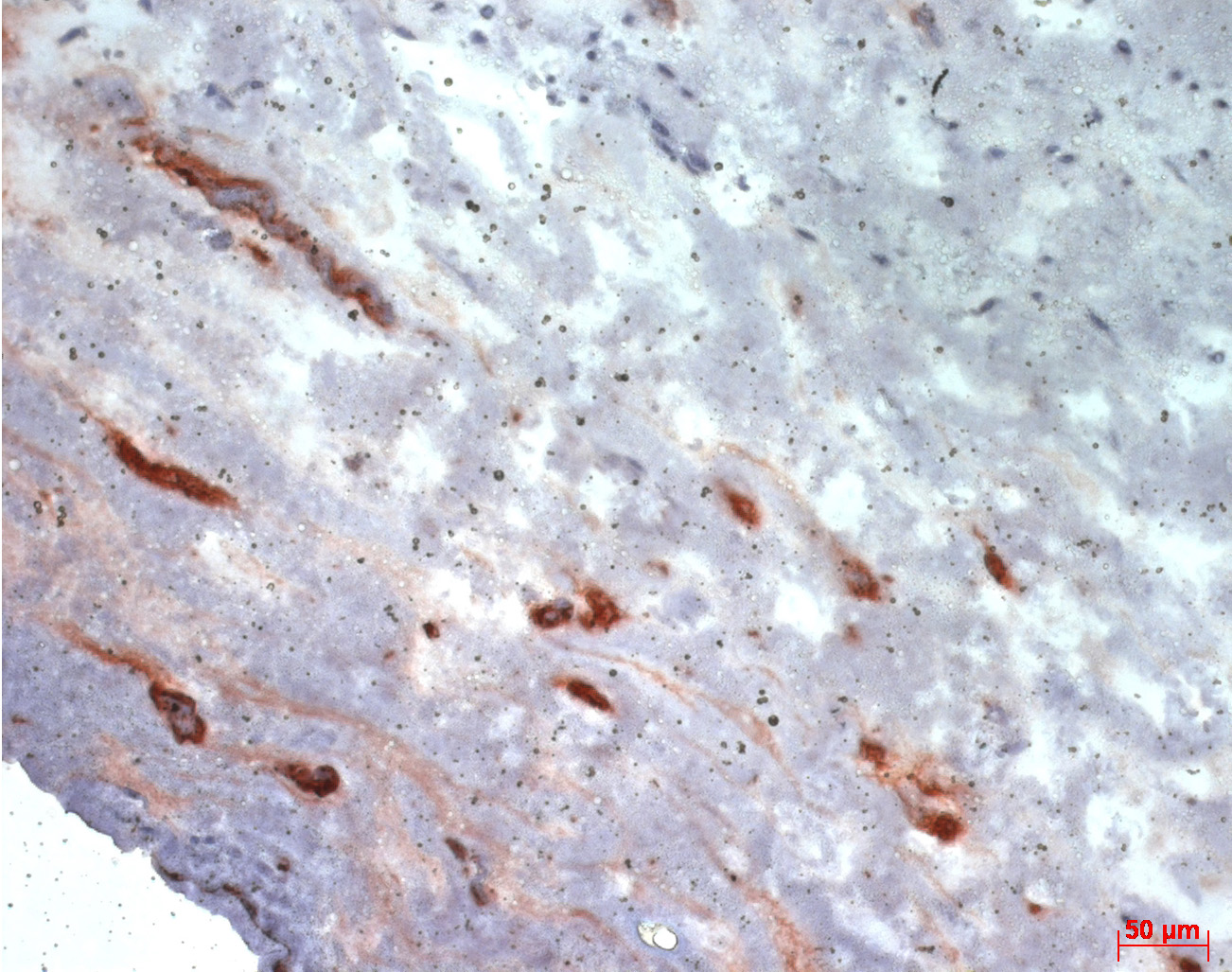
Scientists at the Fraunhofer Institute for Interfacial Engineering and Biotechnology, IGB, have developed a three-dimensional skin equivalent built up of two human cell types: fibroblasts and keratinocytes. Just like natural skin, the in vitro skin has a multi-layered epidermis and an outer horny layer. This 3D skin has been established as a test system, e.g. for testing biocompatibility of new cosmetic or chemical substances. It can also be used for studies of wound healing when an artificial wound is set.
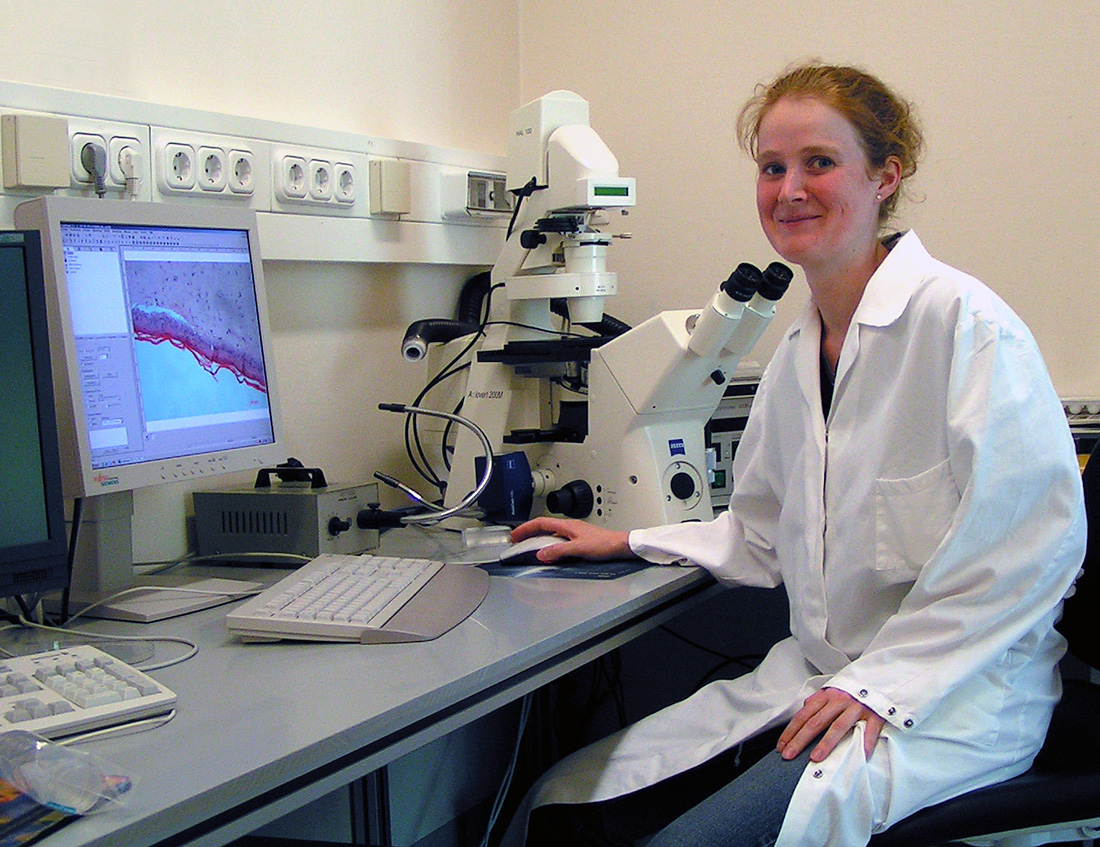
During her research placement at the Fraunhofer IGB, Silke Kersen succeeded to extend the 3D skin model by endothelial cells – the cells which enwrap our blood vessels – and to build up capillary-like structures. “Up to now, the problem has been to stimulate endothelial cells to form capillary structures in their new artificial environment,” explains the winner of the second Hugo-Geiger Prize. “But in the correct mixture with growth factors and two further cell types that form tissue-supporting substances, a 3D network simply grows – without any additional aids.”
Additionally, she integrated melanoma cells into the artificial skin. These skin tumor cells generate exactly those growth factors which stimulate growth of the endothelial cells. Division and migration of endothelial cells hereby could be improved.
“Using our in vitro angiogenesis model we now are able to test angiogenesis inhibitors and investigate if they are suited for tumor therapy”, says Heike Walles, head of the Cell and Tissue Engineering Department at Fraunhofer IGB. “And there is a great advantage compared to conventional models, because our skin is built up of human cells and thus results can easily be transferred to human beings.”
 Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB
Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB