Patching the windpipe
If the human trachea is damaged, doctors can usually do nothing to help. Researchers are cultivating new types of tissue to patch the holes, and which may one day be able to replace entire organs. The tissues are also suitable for use as testing systems for new drugs.
Breath by breath, air forces its way through the windpipe, fills the lungs and flows out again. But if there are holes in the pipe, a large amount of air is lost. Doctors can simply stitch up smaller holes, but larger ones are impeded by cartilaginous rings that hold the muscle tube in place. Physicians are therefore usually helpless when faced with such a respiratory disease. All attempts to patch the trachea with tissue foreign to the body are doomed to failure, as no suitable material has ever yet been found: Plastics are often invaded by pathogenic bacteria. Nor is the immune system deceived by foreign tissues, and they are quickly rejected.
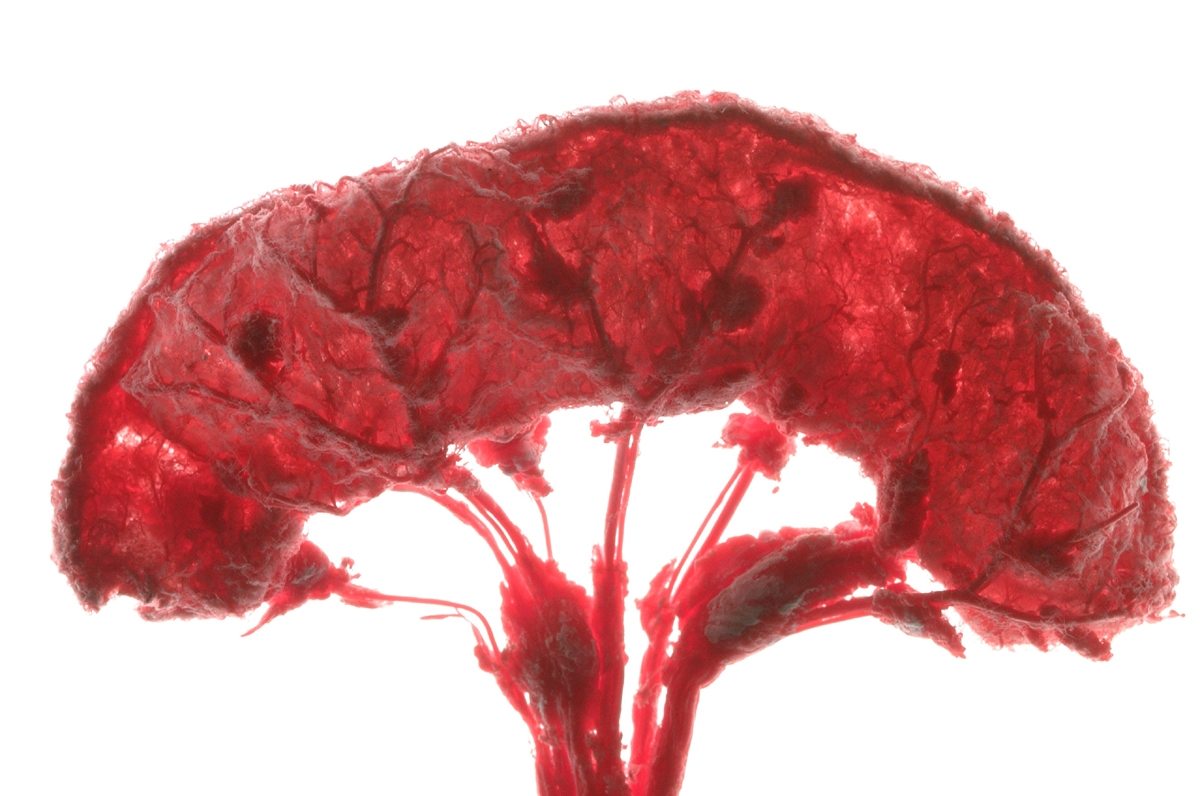
But patients with such afflictions will soon be able to breathe a sigh of relief. “We cultivate human tissue on a pig’s gut from which we have previously removed all animal cells,” explains Professor Heike Walles, who heads the Cell Systems department at the Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB in Stuttgart. “All that is left of the gut is the vascularized matrix – the network of former blood vessels, in fact. We use this as the substrate for endogenous human cells.” Doctors stitched tissue cultivated in this way over the holes in an elderly patient’s trachea – and the result is encouraging: The patch has remained stable, and the body has not so far rejected the new tissue. “Our next step will be to try for successful grafting of large tissue sections, about five centimeters long,” Walles continues. To make this possible, the researchers have created transplant tissue with its own blood supply – vascularized tissue. Whilst blood vessels grow quickly through small pieces of tissue and are able to supply it with blood, this takes too long for larger pieces. Yet without a blood supply of its own, the tissue would very soon die.
The tissue can also be used as a testing system for new drugs. For example, the researchers recreate parts of the liver in the laboratory by cultivating liver cells on the matrix. When they inject drugs into the blood channels of the “organ”, they can study its reaction. “We’ll be using it in pharmaceutical trials from the end of this year,” Walles hopes. “Later, we plan to cultivate extracorporeal support systems for the liver as well.” But first the researchers will have to ensure that the liver performs all its functions reliably and for as long as possible.
 Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB
Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB